Sight Loss Councils communications officer involved in world-first Moorfields project
This week, Sight Loss Council Communications Officer Nicki Guy has featured across national news outlets, speaking openly about her experience of receiving a ground-breaking new treatment for hypotony at Moorfields Eye Hospital in London. Hypotony is a rare condition caused by low eye pressure, which can lead to progressive sight loss.
Nicki’s story has captured widespread national and even international, attention – helping to raise vital awareness of a condition that is often misunderstood and overlooked. Her experience is also highlighting a pioneering treatment that could offer new hope to people affected by hypotony.
Coverage includes being one of the top stories on the BBC national website, as well as appearances on BBC National News, Good Morning Britain News, and in more than 140 media outlets in the UK and globally – a figure that continues to grow.

Nicki pictured during her interview with Sophie Hutchinson at the BBC
A new approach to treating hypotony
The treatment Nicki received is part of a new approach being developed at Moorfields, using a widely‑available eye injection to help manage hypotony. This week, details of the innovative Moorfields project were published in the British Journal of Ophthalmology, showcasing encouraging early results.
Hypotony occurs when the pressure inside the eye becomes abnormally low, altering the eye’s shape and internal structures. Without intervention, this can lead to gradual and sometimes permanent sight loss over a number of years. It often develops in people with underlying eye conditions that affect fluid production inside the eye.
Until now, the main treatment option for sight loss caused by hypotony has been the use of silicone oil to support the eye. While beneficial in some cases, silicone oil is not ideal for long‑term use, as it can be difficult to see through and may cause further complications over time.
This condition is characterised by abnormally low eye pressure, which alters the eye’s normal shape and internal structure. Over time, this can lead to progressive and permanent vision loss, often taking several years to result in blindness. Hypotony may develop as a result of underlying eye conditions that damage the part of the eye responsible for producing the fluid that maintains normal eye pressure.
Until now, the standard treatment for eyes losing vision from low pressure has been to fill them with silicone oil. This has many benefits but is not ideal as it can be toxic to ocular structures over long periods of time and is difficult to see through.
The data published today indicates that eye injections containing HPMC (hydroxypropyl methylcellulose) – a low-cost gel used in most ocular surgery – can be safely used to increase the volume of eyes with hypotony, increasing both their size and pressure.
Remarkably, in addition to restoring ocular anatomy, patients also regained sight. Seven of the eight patients who received the treatment experienced improvements in vision, eye pressure and length restoration after a twelve-month course of treatment. These all came from the world’s first dedicated hypotony clinic, enabled by funding from Moorfields Eye Charity.
Nicki’s story
Nicki’s sight issues began shortly after the birth of her son, when she was diagnosed with uveitis. For several years, she lived symptom-free, until cataracts and further complications began affecting her eyes.
Multiple treatments were attempted, including the use of steroids and silicone oil. While some offered temporary relief, others led to sudden drops in pressure or even complete loss of vision.
Through every challenge, Nicki remained determined to preserve what sight she still had. Losing vision had been frightening, but it also pushed her to find out about treatment options and cutting-edge research.
Nicki was the first patient to have this pioneering treatment, and describes the treatment as ‘life-changing’, saying:
“After I lost vision in my left eye, I thought, ‘there has to be something else we can try’. It felt good that I’d been able to advocate for myself, like they understood my concerns.”
Her turning point came when her consultants at Moorfields began exploring an alternative to silicone oil. Encouraged by her persistence, they trialled a new approach – an injection of clear gel designed to support pressure and restore function.
Reflecting on that moment, Nicki said:
“We went ahead and, as the pressure improved, my vision started to come back. It was incredible!
“I want to keep my eyesight as long as I can, and this gives me that hope, as my sight has slowly returned.
“The progress I’ve made feels extraordinary, especially knowing that patients before me have faced irreversible sight loss.
“I remember seeing Mr Petrushkin and him saying, ‘Before this treatment, people were going blind.’ It’s incredible to know that people are regaining vision.
“I’ve gone from counting fingers and everything being really blurry to being able to see.
“I highly recommend this treatment. Giving people their sight back is something special.”
Moorfields consultant ophthalmologist Harry Petrushkin said:
“We are excited that this simple treatment has proved so effective for patients with this rare condition. This is the start of a process of understanding more about the balance of fluid inside the eye, leading to improved care for our patients.”

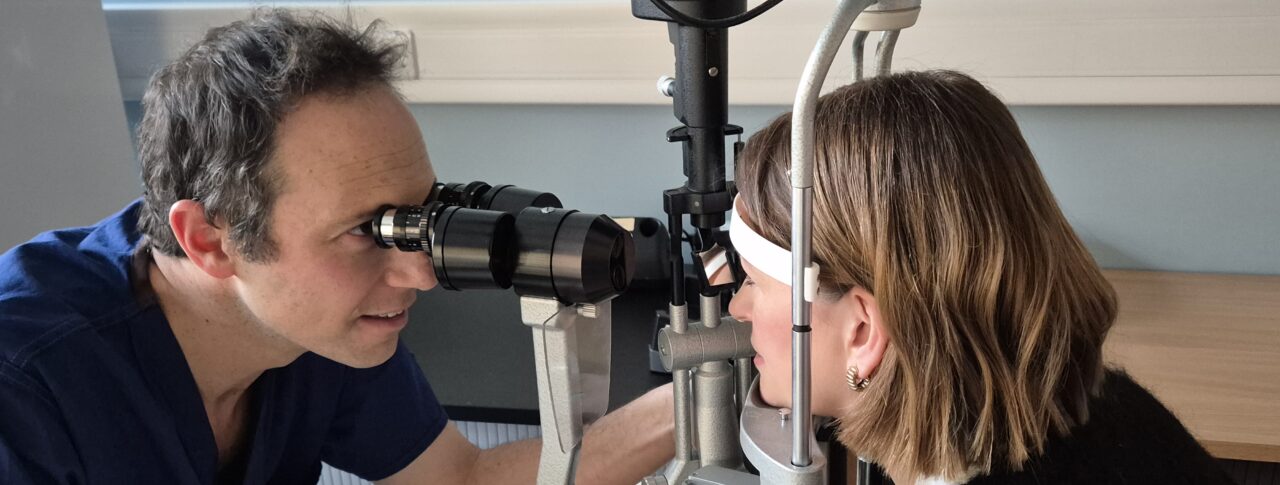
Dr Petrushkin in clinic
The Moorfields clinic integrates structured clinical assessment and collaboration with bioengineers at UCL to understand the drivers of chronic low intraocular pressure.
This preliminary data is already informing thinking on standardised hypotony treatment nationally. It provides a foundation for future, larger-scale formal clinical trials to evaluate the potential of this highly promising approach.
This project could not have taken place without the funding from Moorfields Eye Charity.
Publication date: 15 January 2026